A record
of concern:
The Anderson birth was hardly the first time that
Community Hospitals officials had cause to doubt Morgan's
care.
In 1986, Community put Morgan on a year's probation and
ordered a review of his obstetrical and gynecological
cases after he refused to respond to nurses' complaints
about "medical management of specific cases."
In addition, hospital records show, concern was expressed
about Morgan's "adherence to guidelines and policies"
of the obstetrics and gynecology department. Also
questioned was the physician's manner of communicating
with the nursing staff.
Further, from 1988 to 1990, Morgan had "significant
quality of care issues."
Morgan, in his state deposition, confirmed that Community
Hospitals officials long were uncomfortable with his
medical approach.
He complained that they had scrutinized him since the
1980s.
"They had a magnifying glass out," he said.
Morgan's patients, though, would never know it.
All the hospitals' review proceedings were, as the law
provides, held in private.
Publicly, Community presented Morgan as a doctor in good
standing.
In March 1990 - less than two months after Kyle
Anderson's death - Community included Morgan's name among
hundreds of staff physicians in a newspaper advertisement
marking National Doctors Day.
The headline: "How to recognize a good physician
when you see one."
Three months later, The Indianapolis Star published a
Pulitzer Prize-winning series exposing flaws in the
state's system for disciplining negligent doctors. The
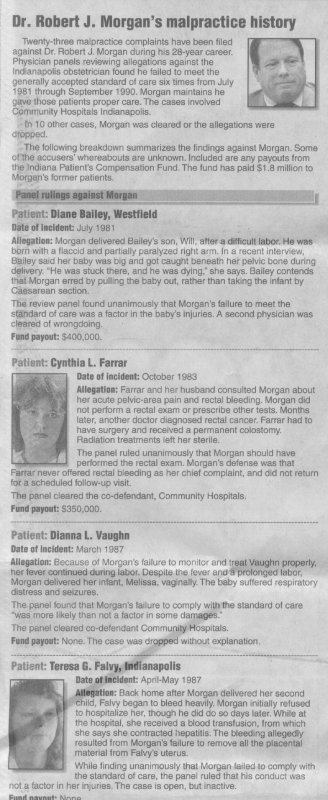
second day of the series led with the case of Cynthia
Farrar.
Farrar and her husband had obtained a malpractice
settlement against Morgan, who they said failed to
perform a routine rectal exam on her when she went to him
in 1983 with complaints of rectal bleeding. Another
doctor later diagnosed cancer.
Cynthia Farrar had to have a permanent colostomy;
radiation treatments left her sterile.
Morgan earlier had lost another malpractice case, The
Star reported.
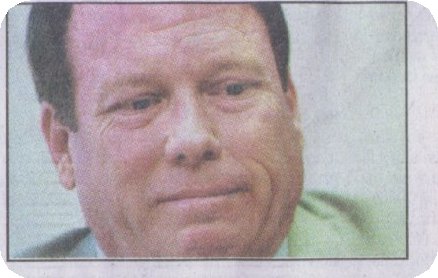
It was shocking news to Rebecca and Douglas Garvin.
A week earlier, they had buried their fourth child.
Going for a run
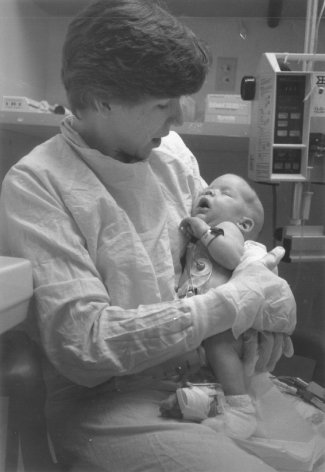
Rebecca Garvin's pregnancy defined high-risk. She had
lost twin sons to prematurity and a third child to
miscarriage.
Morgan, though not Garvin's regular physician, was on
call the night in April 1990 when she had pain.
Over the phone, Garvin related her tragic past and
symptoms. She recalls that Morgan seemed unconcerned and
prescribed no medication.
The next day - hemorrhaging - Garvin went to Community
East. There, Morgan examined her to determine whether she
was dilated. She wasn't. Garvin says he told her that she
was one of the reasons insurance rates were rising and
sent her home.
Another physician subsequently ordered a test to
determine the cause of the bleeding, then put Garvin on
bed rest. But two months later, Garvin, who had a history
of rapid labor, began having contractions.
Now in danger of giving birth just 22 weeks into her
pregnancy, Garvin asked for any physician but Morgan. But
again, only he was available.
Garvin says she was at the hospital at least three hours
before Morgan arrived.
This time, he ordered tests.
Then, Garvin says, Morgan announced that he was going for
a run. "I'll be back later," he said.
Morgan's casual attitude distressed Garvin and her
husband.
"We were fighting for our daughter's life,"
Rebecca Garvin said.
After returning, Morgan gave Garvin drugs to suppress her
contractions, then transferred her to another hospital.
But by then, Garvin had begun to dilate.
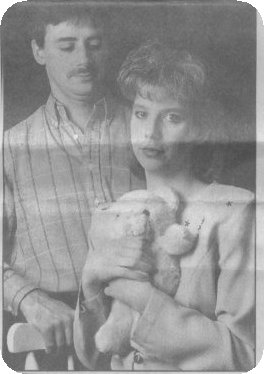
Dark-haired Nicole Linden Garvin, weighing a pound, died
in her parents' arms.
Morgan insists that he gave Garvin the "national
standard of care." But he acknowledges that while
awaiting an ultrasound, he did go for a stress-reducing
run.
"She was one of those cases who was just difficult.
. . . And I ran from the hospital and then ran back,"
he said. Morgan added dryly, "I could have sat in
the doctors' lounge."
The Garvins' baby was so premature that her chances of
survival were poor.
Could the pregnancy have been extended, and Nicole's
chances for survival improved, had Morgan taken her
mother's complaints more seriously?
The Garvins admit they don't know.
But at least, Douglas Garvin said, she would have had
"a fighting chance."
A mother's questions
Myrna Hurless says Morgan didn't take seriously her
complaints of bleeding, either.
During her troubled 1993 pregnancy, Morgan allegedly told
the 17-year-old mother of one that she was too young to
have two kids anyway. Another time, the waitress asked
Morgan whether she should be on bed rest. "No,"
Hurless says Morgan replied. "You'll get fat and
lazy."
Hurless delivered an 11-ounce son, 3 1/2 months early.
The infant lived 48 minutes.
Morgan, who was not present for the delivery, denies poor
prenatal care and says he never made snide comments to
Hurless. Distraught people, he observes, sometimes get
such "things" in their heads.
But in her complaint to the state, Hurless blamed Morgan
for her devastated life.
"Now my son was dead," she wrote, "and I
had a doctor who didn't care."
A
doctor's defense:
To Robert Morgan, all this talk about individual cases
misses the larger point: On average, he says, his
patients have faired better than those of other local
physicians. And, he added, his number of "surgical
interventions" was the lowest around.
"You're looking at little bitty case incidents that
are major to these people," Morgan told a reporter.
"Where you're losing sight is that medicine needs to
change. It needs to reduce costs. (And) it needs to keep
good outcomes."
Morgan says he has delivered more than 3,000 babies, but
that critics unfairly dwell on a relatively few bad
results.
Among medical specialties, obstetrics-gynecology ranks
high for the number of malpractice claims. Nationally,
almost three-quarters of obstetrician-gynecologists have
been accused of negligence at least once; nearly a
quarter have had four claims or more.
Of the 33 malpractice claims filed against Morgan, 10
have been dropped or resolved in his favor.
In other cases, Morgan says, he agreed to settle
malpractice complaints rather than point an incriminating
finger at co-defendants.
Morgan also says that in an act of conscience, he once
warned his patients about a clip he had used in surgeries
that he later determined was faulty. When some patients
turned around and sued him, his malpractice insurer
refused to renew his coverage, he says.
Morgan's next insurer also refused to renew. Again, the
physician says, it was related to his malpractice claims.
Morgan feels picked on by Community Hospitals, too.
He says officials, for example, questioned why he didn't
call a resuscitation team more often. And Community urged
him to be more generous in dispensing epidurals to
laboring women in pain.
But Morgan says he felt better able than most to care for
distressed newborns.
And he maintains that it should be the doctor's call -
not the woman's - whether medications are used.
Epidurals, he says, can interfere with labor, adding that
he needs the patient's cooperation to push. "I can't
have her paralyzed," he says.
Morgan is derisive about "defensive medicine" -
doing procedures partly to guard against negligent
complaints.
"One of the real problems has been that doctors have
to worry about being sued, and . . . I tend not to
practice that way," he said in his state deposition.
"Unfortunately, I'm being reviewed by people who
practice that way, and I'm being critiqued by a hospital
which is very sensitive to adverse publicity."
Morgan says he was even told, "You can't be
different."
Dollars
and deference:
Yet through it all - rising malpractice claims, nurses'
incident reports, internal hospital scrutiny - Morgan
kept working.
And Community Hospitals continued to market him.
Until 3 1/2 years ago, when the hospitals removed him
from the service, Morgan remained on Community's
telephone physician-referral line.
To Lori Rollins' malpractice attorney, Bruce Kehoe, the
reason for Community's deference toward Morgan is clear.
"It's money," he said. "Deliveries going
through the door."
Morgan boasts that he once had "by far" the
largest obstetrical practice in Marion County. And he
says he brought in up to 300 deliveries per year for
Community.
He says he was for years Community's top-producing
obstetrician, "if you want to look at medicine in
those terms, and I assure you that hospitals do."
But Morgan says the hospitals soured on him when
patients' complaints appeared in news stories.
Community Hospitals rejects suggestions that either fear
of bad publicity or Morgan's big practice affected its
actions toward the physician. A doctor's qualifications
to be on staff are judged by panels of other private
physicians who do not benefit from the success of that
doctor's practice, the hospitals say.
And while not disputing Morgan's contention that he was a
high-volume obstetrician, the hospitals add: "This
was many years in the past."
The
scrutiny grows:
Morgan's practice began to unravel in 1995.
Care that he rendered to three patients would trigger
more malpractice claims. And there were additional
incidents, publicly revealed for the first time in the
attorney general's complaint.
Morgan, the complaint said, failed to properly
resuscitate or treat three struggling newborns.
In December 1995, Community East took action to deny
renewal of Morgan's obstetrical privileges and ordered
him to undergo a physician-assessment program in Colorado.
But months later, Community reappointed him with
conditions.
Morgan had to obtain a physician adviser to discuss his
cases, and rectify deficiencies in his patient charts.
Community also ordered Morgan evaluated for disruptive
behavior.
Morgan reduced some of his pregnant patients to tears
when he scolded them about weight gain or did not answer
their questions. His demanding manner also intimidated
some nurses.
One former patient who sued Morgan for malpractice,
Kimberly Cole, says her nurses at Community East seemed
"scared to death of him."
Some made unsettling comments about Morgan.
"Listen," one nurse told Cole and her husband,
"you don't know this doctor."
Particularly concerning to some nurses was Morgan's habit
of laying newborns on their mothers' abdomens after
delivery. Morgan says the technique warms the babies and
bonds them with their mothers.
He contends that concerns arose when nurses at Community
North jumped to the wrong conclusion that some
unresponsive babies needed urgent treatment.
Morgan says newborns sometimes look worse than they are.
They don't need resuscitation, he says, just a bit of
stimulation. After that, he says, it is perfectly safe to
give the baby to Mom.
Morgan rejects the "disruptive" charge as a
"tag" that a Community Hospitals administrator
hung on him.
And he asks sardonically how he could have had such a
large, thriving practice if everyone hated him.
Morgan
certainly has defenders:
Beth Bowles of Indianapolis credits the physician's quick
action with saving her oldest child's life. Her son Chris
was born with a hole in his lung and could not breathe.
So Morgan "immediately went to work on the baby,"
Bowles said. Chris today is a normal, healthy 9-year-old.
Nancie Hicks of Cumberland recalls how Morgan, as she was
going under anesthetic for a surgery, held her hand and
comforted her.
And Elizabeth Abbott of Indianapolis recounts how during
one hospital attempt at labor, Morgan let her remove a
scratchy fetal monitor strip from her abdomen so she
could sleep.
Abbott calls it a "shame" that such a caring
doctor isn't still delivering babies.
Community Hospitals officials privately judged Morgan's
clinical skills "of acceptable quality." They
concluded that some of the malpractice claims and other
complaints may arise from "Dr. Morgan's aggressive,
self-proclaimed `ahead of his time' and nonconventional
approach to the practice of medicine."
Also: "Dr. Morgan's narcissistic and defensive
personality, and his poor documentation of (patient)
histories" might explain the large number of
complaints.
In April 1996, Community Hospitals officials had one more
worry.
They fretted about whether Morgan's medical judgment was
clouded by his "strong desire to minimize the number
of C-sections that he performs." |